
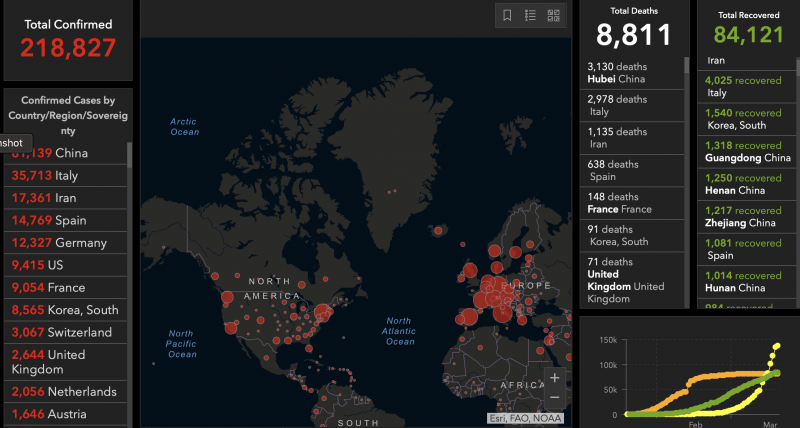
View larger. | Infographic showing global coronavirus cases: 8,811 total deaths and 84,121 recovered as of March 18, 2020. Coronavirus COVID-19 Global Cases via Johns Hopkins University. Check the life chart for updates.
For EarthSky’s most current coronavirus links, click here.
Updated March 23, 2020:
1. The shortage of medical supplies, including personal protective equipment (PPE), continues to dominate COVID-19 news in the U.S.
Health care workers have been turning to social media for supplies: hospitals requesting supplies, organizations asking how they can donate supplies, and individuals organizing collections for hospitals.
PLEASE SHARE: UCSF frontline #covid19 care providers are in urgent need of critical supplies such as masks, disposable gloves & more. You can drop off donations at 3 sites in San Francisco and Oakland starting Monday, 3/23.
More info ?? https://t.co/vwNQwUx12Y #coronavirus pic.twitter.com/1Y8pISHpfA— UC San Francisco (@UCSF) March 22, 2020
Websites are being set up to connect suppliers with hospitals. GetUsPPE.org connects medical institutions needing PPEs with donors. Project N95 is working on a larger scale with state and local governments and manufacturers. There are also other efforts, like this one:
I've setup #PandemicResponseNetwork on the project management site #Basecamp. It's a platform where we can organize efforts by region and share best practices, resources, and suppliers. You can join via this link: https://t.co/CvpTTL2eTY #CoronavirusPandemic #Covid19 #Covid_19
— Dr. Lisa Galarneau ?? ????????????? (@lisaga) March 22, 2020
The government has been working with the private sector to sharply ramp up production of PPEs, but it’s not clear how soon those supplies will be available. The Washington Post reports that governors are increasingly frustrated by the shortage of medical supplies. Currently, states are responsible for their own PPE purchases. But this can lead to them bidding against each other and other inefficiencies in the distribution of supplies. New York governor Andrew Cuomo has asked the Trump administration to nationalize the medical supply chain.
I’m calling on the Federal Government to nationalize the medical supply chain.
The Federal Government should immediately use the Defense Production Act to order companies to make gowns, masks and gloves.
Currently, states are competing against other states for supplies.
— Andrew Cuomo (@NYGovCuomo) March 22, 2020
2. The New York Times reported that a loss of sense of smell (anosmia) and changes to sense of taste (dysgeusia) are also symptoms of COVID-19.
According to the CDC, COVID-19 symptoms appear two to 14 days after exposure. The most common symptoms are fever, cough, and shortness of breath. Serious symptoms requiring emergency treatment are trouble breathing, continual pain or pressure in the chest, confusion or being unable to wake up, and bluish lips or face. (Patients have also reported runny nose, sore throat, headache, muscle aches, and chest tightness.)
The American Academy of Otolaryngology (the medical field specializing in ear and throat conditions), posted a message on their website about the new symptoms:
Anecdotal evidence is rapidly accumulating from sites around the world that anosmia and dysgeusia are significant symptoms associated with the COVID-19 pandemic. Anosmia, in particular, has been seen in patients ultimately testing positive for the coronavirus with no other symptoms. We propose that these symptoms be added to the list of screening tools for possible COVID-19 infection. Anosmia, hyposmia [reduced ability to smell], and dysgeusia in the absence of other respiratory disease such as allergic rhinitis, acute rhinosinusitis, or chronic rhinosinusitis should alert physicians to the possibility of COVID-19 infection and warrant serious consideration for self-isolation and testing of these individuals.
3. In cities severely impacted by COVID-19, such as New York City, medical workers have been under extraordinary stress. Often, they are being forced to reuse masks and gowns. Several have become infected.
In the past few days, some medical workers have posted on Twitter that they are going over advanced directives and wills with their families.
Today broke my heart.
Today I picked up scrubs and repurchased the clogs that got me through residency and fellowship. No more clothes or shoes that go home.
Today I had colleagues get tested for CoVid.
Today I talked about advanced directives with every ICU doctor I know.
1/— RanaAwdishMD (@RanaAwdish) March 22, 2020
Former U.S. surgeon general Vivek Murthy reflected on what his colleagues are going through in this March 23 twitter thread.
It’s 2am and all I can think about is that in hospitals and clinics across America, my friends and colleagues are going to war against #COVID19 with no protection. Would we ever accept sending soldiers into battle without armor? (1/x)
— Vivek Murthy (@vivek_murthy) March 23, 2020
4. This simple animation illustrates how social distancing can cut down on infections.
How much harm can one person really do? A sobering image of just how powerful social distancing can be in fighting COVID-19 #coronavirus pic.twitter.com/AHHcJGNwPH
— Ajit Johnson (@ajitjohnson_n) March 23, 2020
5. A team of data scientists have been working with epidemiologists and public health officials to create a tool that shows how the COVID-19 pandemic affects each state. These models were set up to help states make decisions on their response to the pandemic.
6. The American Red Cross says there is a severe blood shortage due to a large number of blood drive cancellations. Please donate blood, if you are able.
We now face a severe blood shortage due to an unprecedented number of blood drive cancellations during this #coronavirus outbreak. Make an appointment to help patients counting on lifesaving blood: https://t.co/lQdFEVrctc pic.twitter.com/rnUpJF1vq4
— American Red Cross (@RedCross) March 17, 2020
Updated March 20, 2020:
1. There are escalating concerns about the U.S. medical care infrastructure’s ability to handle the COVID-19 outbreak. Hospitals around the country are facing severe shortages of personal protective equipment (PPE) such as masks. Tom Inglesby (@T_Inglesby), of the Johns Hopkins School of Public Health, summarized the dire situation in a post on Twitter, describing not just the lack of PPEs, but also shortages in basic testing equipment. He again expressed concern about an impending shortage of ventilators as more critically ill people are hospitalized. Inglesby wrote on March 19:
We need a massive logistics effort to deal with all of these shortages, and the shortages and material needs that will come. Responsibility shifted to FEMA today. FEMA does have large logistics capability, but their focus is normally on disaster recovery.
The agency best suited for the massive logistics and supply chain operation now needed across the country may be the Defense Logistics Agency.
There are dire shortages of masks around the country – N95 and surgical masks. This
NYT report says doctors and nurses are at war with this virus with no ammo: https://t.co/5LR9IXYlMr 2/x— Tom Inglesby (@T_Inglesby) March 20, 2020
Meanwhile, grassroots efforts continue to help hospitals restock critically needed supplies. Buzzfeed reported on volunteers working to collect and donate supplies to hospitals. Some are innovating new ways to do it, like sewing masks and using 3-D printers to create face shields.
The Washington Post reported that new legislation, enacted on March 18, will allow certain types of N95 masks intended for industrial use, such as construction, to be made available to medical workers. In return, manufacturers will be protected from lawsuits that may arise from the use of these masks.
2. On March 19, Governor Gavin Newsom placed California’s 40 million residents under a stay at home order. A factsheet on the state government’s website says the order is in place until further notice. Essential services remain open: gas stations, pharmacies, food supply stores, banks, and laundry services. Dine-in restaurants, gyms, and other public areas are closed. According to their COVID-19 response website, as of March 18 there were 675 people who have tested positive and 16 deaths. The Los Angeles Times reported that the state projected that as many as 25.5 million people could be infected in California over an eight-week period. The LA Times did not make clear whether that was the estimate “without mitigation” (without social distancing, for example) but it likely is. The extreme social distancing suggested by Governor Newsome is an attempt to lower that projected number.
3. On March 19, New York Governor Andrew Cuomo (@NYGovCuomo) posted an appeal on Twitter for retired health care professionals to sign up as reserve staff in case their help is needed. Data scientist Michael Donnelly has forecasted that New York City hospitals could reach their capacity of about 3,000 cases by March 24. He recommends that Governor Cuomo shut down the city except for essential services.
4. The Hill’s update on coronavirus in the context of U.S. politics, as of March 19, 2020: 14 things to know today about coronavirus. “On Capitol Hill … Senate Republicans released ‘phase three’ of the legislative response to the coronavirus, a $1 trillion economic relief package. Now they’ll look to work with Democrats on a bipartisan bill. Over at the White House, President Trump offered conflicting information about a potentially promising treatment for the COVID-19 disease. He claimed the FDA had approved an old malaria drug to treat patients, but was quickly corrected by his own FDA chief. On the state front, governors are pleading with Trump for more help getting testing kits and medical supplies.” The Hill is listed as highly reliable and politically neutral, skewing slightly to the right, on the latest Media Bias Chart from Ad Fontes Media.
Updated March 19, 2020:
1. The World Health Organization (WHO) is tracking the number of COVID-19 cases by country. As of March 18, 2020, WHO has tracked over 207,860 confirmed cases, and 8,657 deaths, worldwide. Contrast those numbers with the chart above, which is from Johns Hopkins University; they are similar. WHO also maintain a comprehensive body of information about the disease.
2. People exhibiting COVID-19 symptoms should use paracetamol (aka acetaminophen, also known by the brand name Tylenol in the U.S.) instead of ibuprofen (brand name Advil in the U.S.) because the latter may worsen their condition. This claim, originally tweeted by French health minister Oliver Veran on March 14, is now being backed by doctors and scientists.
3. In cities hardest hit by the COVID-19 outbreak, hospitals are facing a severe shortage of critical supplies and there aren’t enough health care workers to care for patients. Journalist Evan Siegfried tweeted about one New York City hospital that does not have enough masks. He also said that doctors and nurses exposed to sick patients are continuing to work, instead of going home to be quarantined, because there aren’t enough of them to care for patients. Writer Holly Figueroa O’Reilly tweeted about a hospital in Seattle where staff are making masks out of office supplies. The New York Times reported on an ongoing shortage of ventilators.
Bill Frist (@bfrist on Twitter), a heart transplant surgeon and former U.S. Senate Majority Leader, posted a video on Twitter saying that the lack of COVID-19 testing is severely hampering efforts to treat patients. He also said that the U.S. must ramp up production of urgently needed supplies and COVID-19 tests, and asked that federal leadership make it a priority.
I'm speaking to providers on the front lines- we are burning thru personal protection equipment (#masks, gowns). We must fire up U.S. production of our own #PPE in mass supply immediately. We need federal leadership to make this a priority TODAY. https://t.co/iBgoproC5T#COVID19
— Bill Frist, M.D. (@bfrist) March 18, 2020
4. The Centers for Disease Control and Prevention (CDC) issued a report that said:
This first preliminary description of outcomes among patients with COVID-19 in the United States indicates that fatality was highest in persons ≥85, ranging from 10% to 27%, followed by 3% to 11% among persons aged 65–84 years, 1% to 3% among persons aged 55-64 years, <1% among persons aged 20–54 years, and no fatalities among persons aged ≤19 years.
The report also contained age distribution snapshots of patients as of March 16, including those who were hospitalized and those who did not survive. These values will evolve as more COVID-19 testing becomes available and more people contract the disease.
5. The World Health Organization (WHO) is launching a multinational effort in drug clinical trials to aggressively combat COVID-19. In an article at the website statnews.com, Helen Branswell wrote:
The four drugs or combinations will be compared to what is called standard of care – the regular support hospitals treating these patients use now, such as supplementary oxygen when needed.
The drugs to be tested are the antiviral drug remdesivir; a combination of two HIV drugs, lopinavir and ritonavir; lopinavir and ritonavir plus interferon beta; and the antimalarial drug chloroquine. All show some evidence of effectiveness against the SARS-CoV 2 virus, which causes Covid-19, either in vitro and/or animal studies.
She also noted in a tweet that after the WHO announcement was made, a study on critically ill patients in China was published that showed no improvement in survival or recovery speed for patients taking the lopinavir-ritonavir combination when compared to those under conventional care.
6. The most effective way to combat COVID-19 is with a vaccine. But scientists say it could take as long as 18 months to come up with a safe vaccine, and they would then face the enormous challenge of manufacturing it for billions of people across the world. Until a vaccine becomes widely available, social distancing is the best way to avoid infection. Yale University’s Akiko Iwasaki posted an infographic created by the company BioRender that compares the effectiveness of vaccines and social distancing.
There is a lot of talk about #herdimmunity. Vaccination is the only safe way to achieve it. In the absence of vaccine, we need to practice #SocialDistancing. @BioRender made this amazing infographic to explain how a hypothetical virus spreads through the population. (1/n) pic.twitter.com/ifFspJ80N8
— Prof. Akiko Iwasaki (@VirusesImmunity) March 18, 2020
7. The Hill’s update on coronavirus in the context of U.S. politics, as of March 18, 2020: 15 things to know today about coronavirus. “There are over 7,700 cases of coronavirus in the U.S., according to Johns Hopkins University, and at least 118 deaths. President Trump today invoked the Defense Production Act, which gives the administration the authority to ramp up domestic manufacturing of personal protective equipment and other items needed to fight the coronavirus. Meanwhile in Congress, the Senate passed the House’s amended coronavirus aid package, but GOP senators are already racing to craft the next stimulus package with $1 trillion.” The Hill is listed as highly reliable and politically neutral, skewing slightly to the right, on the latest Media Bias Chart from Ad Fontes Media.

Image via @Laurie_Garrett
Updated March 18, 2020:
1. From the U.S. National Institutes of Health (NIH) on March 17 … How long is SARS-CoV-2 stable on surfaces? “The virus that causes coronavirus disease 2019 (COVID-19) is stable for several hours to days in aerosols and on surfaces …
detectable in aerosols for up to three hours, up to four hours on copper, up to 24 hours on cardboard and up to two to three days on plastic and stainless steel.”
2. From Francois Balloux (@BallouxFrancois on Twitter), a computational biologist at University College London, on March 17 … An analysis of the report by the Imperial College COVID-19 Response team. The report, released on March 16, is here. It suggested the possibility of more than 2 million deaths in the U.S., and half a million deaths in the U.K., if no mitigation efforts were implemented.
3. From physician-scientist Eric Topal (@EricTopol on Twitter) on March 17 … Two plots showing the rate of deaths and rate of new confirmed cases for different countries. Note that the rate of confirmed cases (second plot) is low for the U.S. because not enough test kits are available. There have been many reports of doctors not being able to test people exhibiting classic symptoms of COVID-19 because patients don’t meet testing requirements, specifically that they were in contact with someone who tested positive for the virus.
4. Another one from @EricTopol on March 17 … A Twitter thread that summarizes why testing is important and what it tells us about disease transmission. Widespread testing, like that done in South Korea, showed that the virus is being spread by people who do not display symptoms.
5. A third one from @EricTopol on March 16 … How the lack of test kits is the biggest breakdown in the U.S. response to COVID-19. A histogram of testing in the U.S. vs. South Korea shows how rapidly S. Korea responded with testing, which, with contact tracing, has since helped in a decline in new cases. Both countries detected COVID-19 cases around the same time.
6. From infectious diseases reporter Helen Branswell (@HelenBranswell on Twitter) of @statnews … A look at COVID-19 in Italy as of March 15 – March 17
7. From Tom Inglesby (@T_Inglesby on Twitter), Director, Johns Hopkins SPH Center for Health Security on March 16 … There is a shortage of ventilators in the U.S.
8. From Emory University epidemiologist and health services researcher Rachel Patzer (@RachelPatzerPhD on Twitter) on March 16 … How the pandemic affects doctors: one family’s story
9. From The Hill on March 17 … 12 things to know today about the coronavirus outbreak … a daily roundup of U.S.-based news about the coronavirus, mostly as it relates to U.S. politics. The Hill is listed as highly reliable and politically neutral, skewing slightly to the right, on the latest Media Bias Chart from Ad Fontes Media. According to The Hill‘s March 17 report: “There are 5,894 known cases in the U.S., including 97 deaths [Editor’s note: that number is now greater than 100], according to Johns Hopkins University. The Trump administration wants to send checks to every American in an effort to try to blunt the worst of the economic impact from the coronavirus outbreak – but that might run into problems with Senate Republicans, who are frustrated that they were largely left out of the negotiations on the most recent House-passed bill. Meanwhile, frontline health workers are running out of protective supplies, and states say they are not getting the help they need from the federal government. The Pentagon says it’s willing to help, but it will only be a temporary solution.”
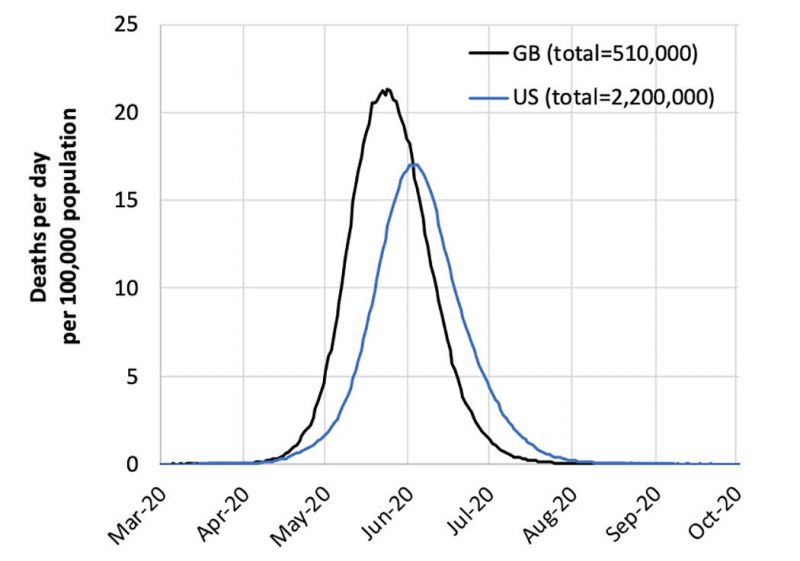
A new report from Imperiod College London shows the number of deaths that could occur in the U.S. and Britain in the absence of actions to control the coronavirus epidemic. Image Imperial College COVID-19 Response Team/ New York Times.
Artist’s depiction of coronavirus, which is a class of viruses that cause respiratory infection in humans and which resemble a crown when viewed under an electron microscope. Image via the CDC.
Updated March 17, 2020:
The New York Times reported Monday on new guidelines issued at a White House press conference. The guidelines were influenced by a new paper from Imperial College London, a modeling study of various possible outcomes of the spread of coronavirus, using suppression and/or mitigation. It’s a long paper, but its summary is digestible. The NY Times sums it up: “To curb the epidemic, there would need to be drastic restrictions on work, school and social gatherings for periods of time until a vaccine was available, which could take 18 months, according to the report, compiled by British researchers. They cautioned that such steps carried enormous costs that could also affect people’s health, but concluded they were ‘the only viable strategy at the current time.'”
Twitter threads discussing the Imperial College London paper:
Thread from March 16, from science journalist and molecular biologist Kai Kupferschmidt (@kakape on Twitter).
Thread from March 17, from public health specialist Amanda Makulec (@abmakulec) of @DataVizDC in Washington, D.C.
Late in the day on Monday, March 16, The Hill – a source we consider to be as politically neutral as any – released the following story. It focuses on Monday’s news of the day, as related to coronavirus: 12 things to know today about coronavirus.
Here’s a research paper in the journal Science about people without symptoms driving spread of virus, from March 16: Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2)
A Twitter thread discussing the Science paper from March 16, from physician-scientist Eric Topal (@EricTopol)
When Idris Elba made his announcement on March 16 that he has the virus, he also pointed out that people not showing symptoms are spreading it.
More from Twitter:
What we should expect as the epidemic unfolds by veteran health reporter and Pulitzer Prize winner Laurie Garrett (@Laurie_Garrett), from March 16.
What to expect as the epidemic unfolds from Andy Slavitt (@ASlavitt), former Acting Administrator of the Centers for Medicare and Medicaid Services, from March 15.
Global situation reports from the World Health Organization (WHO), updated most recently on March 16:
Coronavirus disease (COVID-2019) situation reports
U.S. situation reports from the U.S. Centers for Disease Control (CDC), updated most recently on March 15..
Also from the CDC:
From the CDC, a simple downloadable fact sheet with good basic information about the virus: Coronavirus disease 2019 (COVID-19) and you
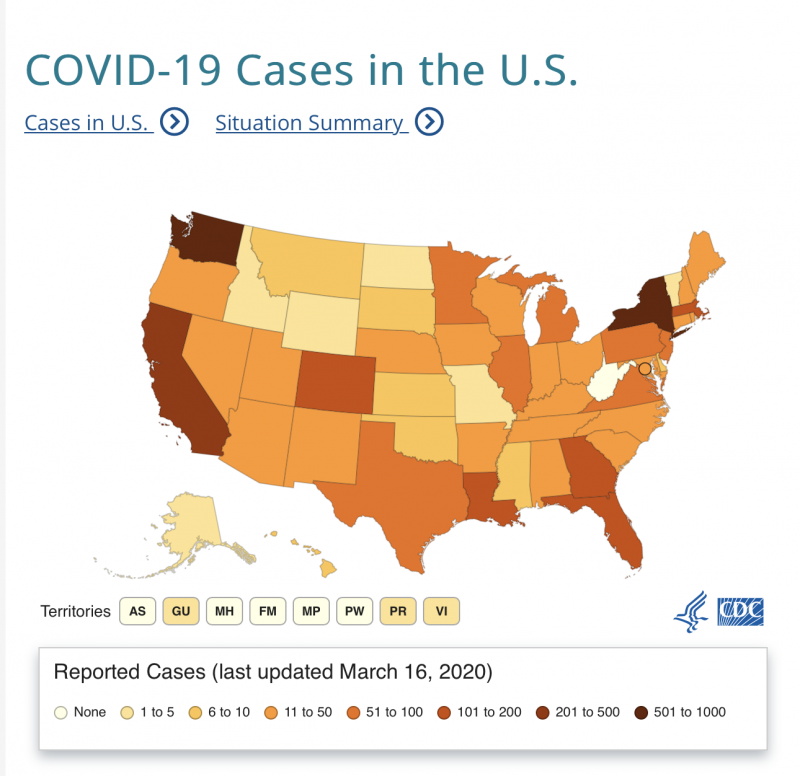
U.S. map showing number of coronavirus cases reported, state by state, as of March 16, 2020. Map via the CDC. (As of March 18, cases have occurred in all 50 states).
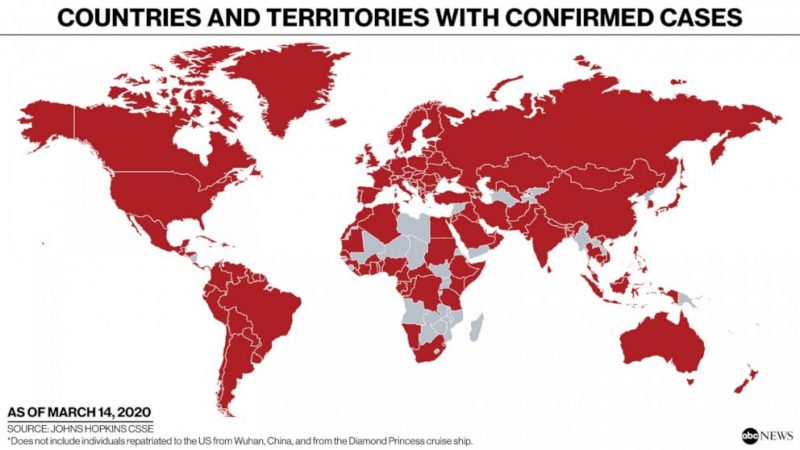
Countries and territories with confirmed cases of coronavirus, as of March 14, 2020. Read more from ABC News: Tracking the spread of coronavirus in the U.S. and around the world. Image via ABC News / Johns Hopkins CSSE.
Some background articles on the virus and its mitigation:
Why does soap work so well on the Sars-CoV-2, the coronavirus and indeed most viruses? Read more from chemist Pall Thordarson, via The Guardian: Here’s how soap kills the coronavirus
As the coronavirus spreads into more and more communities, public health officials are placing responsibility on individuals to help slow the pandemic. A physician explains how social distancing works. Read more from Thomas Perls, Professor of Medicine at Boston University: Why social distancing is the best tool to fight the coronavirus
More interesting threads from Twitter – March 15 and 16 – on the effect of coronavirus test shortages on doctors in the U.S., and how U.S. doctors are coping:
From @DrRobDavidson … Why testing is important from an emergency room doc’s perspective
From @Craig_A_Spencer … Another doctor’s comments, in New York City
From @Vivek_Murthy, who served as 19th Surgeon General in the U.S. … Another perspective (from March 13)
Last but not least, a good video on how social distancing works, using matches.

#StayHome. Image via @ASlavitt.
Bottom line: Links to information on coronavirus, updated March 18, 2020.
from EarthSky https://ift.tt/2UF0huy

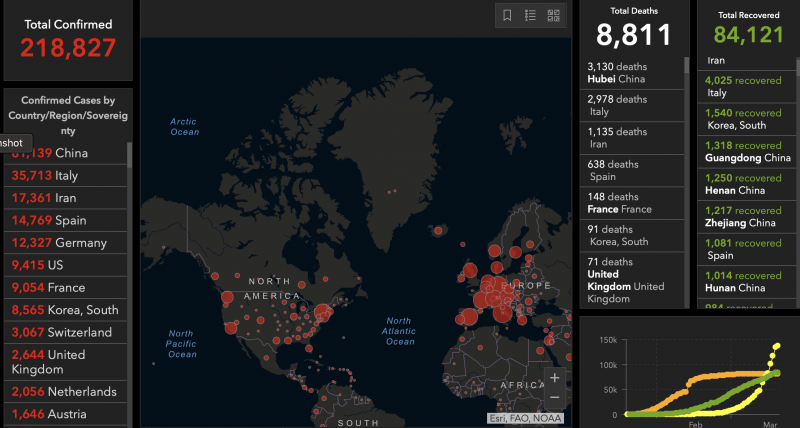
View larger. | Infographic showing global coronavirus cases: 8,811 total deaths and 84,121 recovered as of March 18, 2020. Coronavirus COVID-19 Global Cases via Johns Hopkins University. Check the life chart for updates.
For EarthSky’s most current coronavirus links, click here.
Updated March 23, 2020:
1. The shortage of medical supplies, including personal protective equipment (PPE), continues to dominate COVID-19 news in the U.S.
Health care workers have been turning to social media for supplies: hospitals requesting supplies, organizations asking how they can donate supplies, and individuals organizing collections for hospitals.
PLEASE SHARE: UCSF frontline #covid19 care providers are in urgent need of critical supplies such as masks, disposable gloves & more. You can drop off donations at 3 sites in San Francisco and Oakland starting Monday, 3/23.
More info ?? https://t.co/vwNQwUx12Y #coronavirus pic.twitter.com/1Y8pISHpfA— UC San Francisco (@UCSF) March 22, 2020
Websites are being set up to connect suppliers with hospitals. GetUsPPE.org connects medical institutions needing PPEs with donors. Project N95 is working on a larger scale with state and local governments and manufacturers. There are also other efforts, like this one:
I've setup #PandemicResponseNetwork on the project management site #Basecamp. It's a platform where we can organize efforts by region and share best practices, resources, and suppliers. You can join via this link: https://t.co/CvpTTL2eTY #CoronavirusPandemic #Covid19 #Covid_19
— Dr. Lisa Galarneau ?? ????????????? (@lisaga) March 22, 2020
The government has been working with the private sector to sharply ramp up production of PPEs, but it’s not clear how soon those supplies will be available. The Washington Post reports that governors are increasingly frustrated by the shortage of medical supplies. Currently, states are responsible for their own PPE purchases. But this can lead to them bidding against each other and other inefficiencies in the distribution of supplies. New York governor Andrew Cuomo has asked the Trump administration to nationalize the medical supply chain.
I’m calling on the Federal Government to nationalize the medical supply chain.
The Federal Government should immediately use the Defense Production Act to order companies to make gowns, masks and gloves.
Currently, states are competing against other states for supplies.
— Andrew Cuomo (@NYGovCuomo) March 22, 2020
2. The New York Times reported that a loss of sense of smell (anosmia) and changes to sense of taste (dysgeusia) are also symptoms of COVID-19.
According to the CDC, COVID-19 symptoms appear two to 14 days after exposure. The most common symptoms are fever, cough, and shortness of breath. Serious symptoms requiring emergency treatment are trouble breathing, continual pain or pressure in the chest, confusion or being unable to wake up, and bluish lips or face. (Patients have also reported runny nose, sore throat, headache, muscle aches, and chest tightness.)
The American Academy of Otolaryngology (the medical field specializing in ear and throat conditions), posted a message on their website about the new symptoms:
Anecdotal evidence is rapidly accumulating from sites around the world that anosmia and dysgeusia are significant symptoms associated with the COVID-19 pandemic. Anosmia, in particular, has been seen in patients ultimately testing positive for the coronavirus with no other symptoms. We propose that these symptoms be added to the list of screening tools for possible COVID-19 infection. Anosmia, hyposmia [reduced ability to smell], and dysgeusia in the absence of other respiratory disease such as allergic rhinitis, acute rhinosinusitis, or chronic rhinosinusitis should alert physicians to the possibility of COVID-19 infection and warrant serious consideration for self-isolation and testing of these individuals.
3. In cities severely impacted by COVID-19, such as New York City, medical workers have been under extraordinary stress. Often, they are being forced to reuse masks and gowns. Several have become infected.
In the past few days, some medical workers have posted on Twitter that they are going over advanced directives and wills with their families.
Today broke my heart.
Today I picked up scrubs and repurchased the clogs that got me through residency and fellowship. No more clothes or shoes that go home.
Today I had colleagues get tested for CoVid.
Today I talked about advanced directives with every ICU doctor I know.
1/— RanaAwdishMD (@RanaAwdish) March 22, 2020
Former U.S. surgeon general Vivek Murthy reflected on what his colleagues are going through in this March 23 twitter thread.
It’s 2am and all I can think about is that in hospitals and clinics across America, my friends and colleagues are going to war against #COVID19 with no protection. Would we ever accept sending soldiers into battle without armor? (1/x)
— Vivek Murthy (@vivek_murthy) March 23, 2020
4. This simple animation illustrates how social distancing can cut down on infections.
How much harm can one person really do? A sobering image of just how powerful social distancing can be in fighting COVID-19 #coronavirus pic.twitter.com/AHHcJGNwPH
— Ajit Johnson (@ajitjohnson_n) March 23, 2020
5. A team of data scientists have been working with epidemiologists and public health officials to create a tool that shows how the COVID-19 pandemic affects each state. These models were set up to help states make decisions on their response to the pandemic.
6. The American Red Cross says there is a severe blood shortage due to a large number of blood drive cancellations. Please donate blood, if you are able.
We now face a severe blood shortage due to an unprecedented number of blood drive cancellations during this #coronavirus outbreak. Make an appointment to help patients counting on lifesaving blood: https://t.co/lQdFEVrctc pic.twitter.com/rnUpJF1vq4
— American Red Cross (@RedCross) March 17, 2020
Updated March 20, 2020:
1. There are escalating concerns about the U.S. medical care infrastructure’s ability to handle the COVID-19 outbreak. Hospitals around the country are facing severe shortages of personal protective equipment (PPE) such as masks. Tom Inglesby (@T_Inglesby), of the Johns Hopkins School of Public Health, summarized the dire situation in a post on Twitter, describing not just the lack of PPEs, but also shortages in basic testing equipment. He again expressed concern about an impending shortage of ventilators as more critically ill people are hospitalized. Inglesby wrote on March 19:
We need a massive logistics effort to deal with all of these shortages, and the shortages and material needs that will come. Responsibility shifted to FEMA today. FEMA does have large logistics capability, but their focus is normally on disaster recovery.
The agency best suited for the massive logistics and supply chain operation now needed across the country may be the Defense Logistics Agency.
There are dire shortages of masks around the country – N95 and surgical masks. This
NYT report says doctors and nurses are at war with this virus with no ammo: https://t.co/5LR9IXYlMr 2/x— Tom Inglesby (@T_Inglesby) March 20, 2020
Meanwhile, grassroots efforts continue to help hospitals restock critically needed supplies. Buzzfeed reported on volunteers working to collect and donate supplies to hospitals. Some are innovating new ways to do it, like sewing masks and using 3-D printers to create face shields.
The Washington Post reported that new legislation, enacted on March 18, will allow certain types of N95 masks intended for industrial use, such as construction, to be made available to medical workers. In return, manufacturers will be protected from lawsuits that may arise from the use of these masks.
2. On March 19, Governor Gavin Newsom placed California’s 40 million residents under a stay at home order. A factsheet on the state government’s website says the order is in place until further notice. Essential services remain open: gas stations, pharmacies, food supply stores, banks, and laundry services. Dine-in restaurants, gyms, and other public areas are closed. According to their COVID-19 response website, as of March 18 there were 675 people who have tested positive and 16 deaths. The Los Angeles Times reported that the state projected that as many as 25.5 million people could be infected in California over an eight-week period. The LA Times did not make clear whether that was the estimate “without mitigation” (without social distancing, for example) but it likely is. The extreme social distancing suggested by Governor Newsome is an attempt to lower that projected number.
3. On March 19, New York Governor Andrew Cuomo (@NYGovCuomo) posted an appeal on Twitter for retired health care professionals to sign up as reserve staff in case their help is needed. Data scientist Michael Donnelly has forecasted that New York City hospitals could reach their capacity of about 3,000 cases by March 24. He recommends that Governor Cuomo shut down the city except for essential services.
4. The Hill’s update on coronavirus in the context of U.S. politics, as of March 19, 2020: 14 things to know today about coronavirus. “On Capitol Hill … Senate Republicans released ‘phase three’ of the legislative response to the coronavirus, a $1 trillion economic relief package. Now they’ll look to work with Democrats on a bipartisan bill. Over at the White House, President Trump offered conflicting information about a potentially promising treatment for the COVID-19 disease. He claimed the FDA had approved an old malaria drug to treat patients, but was quickly corrected by his own FDA chief. On the state front, governors are pleading with Trump for more help getting testing kits and medical supplies.” The Hill is listed as highly reliable and politically neutral, skewing slightly to the right, on the latest Media Bias Chart from Ad Fontes Media.
Updated March 19, 2020:
1. The World Health Organization (WHO) is tracking the number of COVID-19 cases by country. As of March 18, 2020, WHO has tracked over 207,860 confirmed cases, and 8,657 deaths, worldwide. Contrast those numbers with the chart above, which is from Johns Hopkins University; they are similar. WHO also maintain a comprehensive body of information about the disease.
2. People exhibiting COVID-19 symptoms should use paracetamol (aka acetaminophen, also known by the brand name Tylenol in the U.S.) instead of ibuprofen (brand name Advil in the U.S.) because the latter may worsen their condition. This claim, originally tweeted by French health minister Oliver Veran on March 14, is now being backed by doctors and scientists.
3. In cities hardest hit by the COVID-19 outbreak, hospitals are facing a severe shortage of critical supplies and there aren’t enough health care workers to care for patients. Journalist Evan Siegfried tweeted about one New York City hospital that does not have enough masks. He also said that doctors and nurses exposed to sick patients are continuing to work, instead of going home to be quarantined, because there aren’t enough of them to care for patients. Writer Holly Figueroa O’Reilly tweeted about a hospital in Seattle where staff are making masks out of office supplies. The New York Times reported on an ongoing shortage of ventilators.
Bill Frist (@bfrist on Twitter), a heart transplant surgeon and former U.S. Senate Majority Leader, posted a video on Twitter saying that the lack of COVID-19 testing is severely hampering efforts to treat patients. He also said that the U.S. must ramp up production of urgently needed supplies and COVID-19 tests, and asked that federal leadership make it a priority.
I'm speaking to providers on the front lines- we are burning thru personal protection equipment (#masks, gowns). We must fire up U.S. production of our own #PPE in mass supply immediately. We need federal leadership to make this a priority TODAY. https://t.co/iBgoproC5T#COVID19
— Bill Frist, M.D. (@bfrist) March 18, 2020
4. The Centers for Disease Control and Prevention (CDC) issued a report that said:
This first preliminary description of outcomes among patients with COVID-19 in the United States indicates that fatality was highest in persons ≥85, ranging from 10% to 27%, followed by 3% to 11% among persons aged 65–84 years, 1% to 3% among persons aged 55-64 years, <1% among persons aged 20–54 years, and no fatalities among persons aged ≤19 years.
The report also contained age distribution snapshots of patients as of March 16, including those who were hospitalized and those who did not survive. These values will evolve as more COVID-19 testing becomes available and more people contract the disease.
5. The World Health Organization (WHO) is launching a multinational effort in drug clinical trials to aggressively combat COVID-19. In an article at the website statnews.com, Helen Branswell wrote:
The four drugs or combinations will be compared to what is called standard of care – the regular support hospitals treating these patients use now, such as supplementary oxygen when needed.
The drugs to be tested are the antiviral drug remdesivir; a combination of two HIV drugs, lopinavir and ritonavir; lopinavir and ritonavir plus interferon beta; and the antimalarial drug chloroquine. All show some evidence of effectiveness against the SARS-CoV 2 virus, which causes Covid-19, either in vitro and/or animal studies.
She also noted in a tweet that after the WHO announcement was made, a study on critically ill patients in China was published that showed no improvement in survival or recovery speed for patients taking the lopinavir-ritonavir combination when compared to those under conventional care.
6. The most effective way to combat COVID-19 is with a vaccine. But scientists say it could take as long as 18 months to come up with a safe vaccine, and they would then face the enormous challenge of manufacturing it for billions of people across the world. Until a vaccine becomes widely available, social distancing is the best way to avoid infection. Yale University’s Akiko Iwasaki posted an infographic created by the company BioRender that compares the effectiveness of vaccines and social distancing.
There is a lot of talk about #herdimmunity. Vaccination is the only safe way to achieve it. In the absence of vaccine, we need to practice #SocialDistancing. @BioRender made this amazing infographic to explain how a hypothetical virus spreads through the population. (1/n) pic.twitter.com/ifFspJ80N8
— Prof. Akiko Iwasaki (@VirusesImmunity) March 18, 2020
7. The Hill’s update on coronavirus in the context of U.S. politics, as of March 18, 2020: 15 things to know today about coronavirus. “There are over 7,700 cases of coronavirus in the U.S., according to Johns Hopkins University, and at least 118 deaths. President Trump today invoked the Defense Production Act, which gives the administration the authority to ramp up domestic manufacturing of personal protective equipment and other items needed to fight the coronavirus. Meanwhile in Congress, the Senate passed the House’s amended coronavirus aid package, but GOP senators are already racing to craft the next stimulus package with $1 trillion.” The Hill is listed as highly reliable and politically neutral, skewing slightly to the right, on the latest Media Bias Chart from Ad Fontes Media.

Image via @Laurie_Garrett
Updated March 18, 2020:
1. From the U.S. National Institutes of Health (NIH) on March 17 … How long is SARS-CoV-2 stable on surfaces? “The virus that causes coronavirus disease 2019 (COVID-19) is stable for several hours to days in aerosols and on surfaces …
detectable in aerosols for up to three hours, up to four hours on copper, up to 24 hours on cardboard and up to two to three days on plastic and stainless steel.”
2. From Francois Balloux (@BallouxFrancois on Twitter), a computational biologist at University College London, on March 17 … An analysis of the report by the Imperial College COVID-19 Response team. The report, released on March 16, is here. It suggested the possibility of more than 2 million deaths in the U.S., and half a million deaths in the U.K., if no mitigation efforts were implemented.
3. From physician-scientist Eric Topal (@EricTopol on Twitter) on March 17 … Two plots showing the rate of deaths and rate of new confirmed cases for different countries. Note that the rate of confirmed cases (second plot) is low for the U.S. because not enough test kits are available. There have been many reports of doctors not being able to test people exhibiting classic symptoms of COVID-19 because patients don’t meet testing requirements, specifically that they were in contact with someone who tested positive for the virus.
4. Another one from @EricTopol on March 17 … A Twitter thread that summarizes why testing is important and what it tells us about disease transmission. Widespread testing, like that done in South Korea, showed that the virus is being spread by people who do not display symptoms.
5. A third one from @EricTopol on March 16 … How the lack of test kits is the biggest breakdown in the U.S. response to COVID-19. A histogram of testing in the U.S. vs. South Korea shows how rapidly S. Korea responded with testing, which, with contact tracing, has since helped in a decline in new cases. Both countries detected COVID-19 cases around the same time.
6. From infectious diseases reporter Helen Branswell (@HelenBranswell on Twitter) of @statnews … A look at COVID-19 in Italy as of March 15 – March 17
7. From Tom Inglesby (@T_Inglesby on Twitter), Director, Johns Hopkins SPH Center for Health Security on March 16 … There is a shortage of ventilators in the U.S.
8. From Emory University epidemiologist and health services researcher Rachel Patzer (@RachelPatzerPhD on Twitter) on March 16 … How the pandemic affects doctors: one family’s story
9. From The Hill on March 17 … 12 things to know today about the coronavirus outbreak … a daily roundup of U.S.-based news about the coronavirus, mostly as it relates to U.S. politics. The Hill is listed as highly reliable and politically neutral, skewing slightly to the right, on the latest Media Bias Chart from Ad Fontes Media. According to The Hill‘s March 17 report: “There are 5,894 known cases in the U.S., including 97 deaths [Editor’s note: that number is now greater than 100], according to Johns Hopkins University. The Trump administration wants to send checks to every American in an effort to try to blunt the worst of the economic impact from the coronavirus outbreak – but that might run into problems with Senate Republicans, who are frustrated that they were largely left out of the negotiations on the most recent House-passed bill. Meanwhile, frontline health workers are running out of protective supplies, and states say they are not getting the help they need from the federal government. The Pentagon says it’s willing to help, but it will only be a temporary solution.”
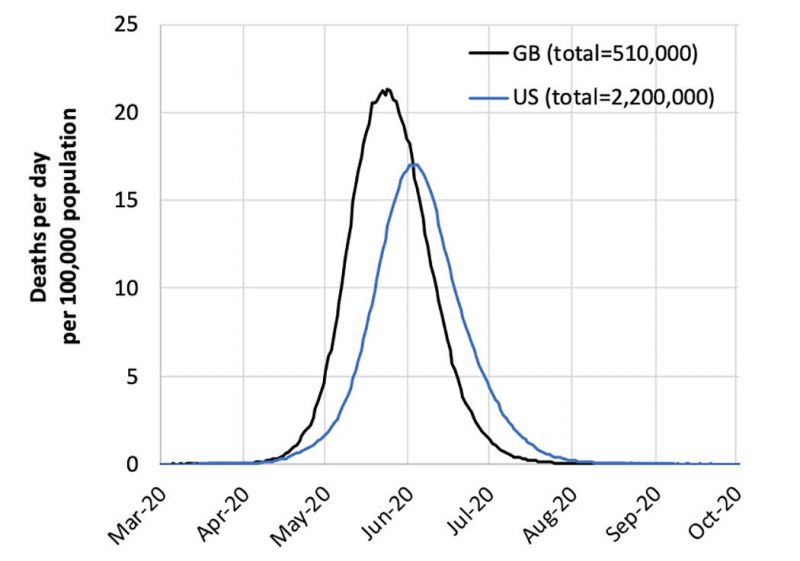
A new report from Imperiod College London shows the number of deaths that could occur in the U.S. and Britain in the absence of actions to control the coronavirus epidemic. Image Imperial College COVID-19 Response Team/ New York Times.
Artist’s depiction of coronavirus, which is a class of viruses that cause respiratory infection in humans and which resemble a crown when viewed under an electron microscope. Image via the CDC.
Updated March 17, 2020:
The New York Times reported Monday on new guidelines issued at a White House press conference. The guidelines were influenced by a new paper from Imperial College London, a modeling study of various possible outcomes of the spread of coronavirus, using suppression and/or mitigation. It’s a long paper, but its summary is digestible. The NY Times sums it up: “To curb the epidemic, there would need to be drastic restrictions on work, school and social gatherings for periods of time until a vaccine was available, which could take 18 months, according to the report, compiled by British researchers. They cautioned that such steps carried enormous costs that could also affect people’s health, but concluded they were ‘the only viable strategy at the current time.'”
Twitter threads discussing the Imperial College London paper:
Thread from March 16, from science journalist and molecular biologist Kai Kupferschmidt (@kakape on Twitter).
Thread from March 17, from public health specialist Amanda Makulec (@abmakulec) of @DataVizDC in Washington, D.C.
Late in the day on Monday, March 16, The Hill – a source we consider to be as politically neutral as any – released the following story. It focuses on Monday’s news of the day, as related to coronavirus: 12 things to know today about coronavirus.
Here’s a research paper in the journal Science about people without symptoms driving spread of virus, from March 16: Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2)
A Twitter thread discussing the Science paper from March 16, from physician-scientist Eric Topal (@EricTopol)
When Idris Elba made his announcement on March 16 that he has the virus, he also pointed out that people not showing symptoms are spreading it.
More from Twitter:
What we should expect as the epidemic unfolds by veteran health reporter and Pulitzer Prize winner Laurie Garrett (@Laurie_Garrett), from March 16.
What to expect as the epidemic unfolds from Andy Slavitt (@ASlavitt), former Acting Administrator of the Centers for Medicare and Medicaid Services, from March 15.
Global situation reports from the World Health Organization (WHO), updated most recently on March 16:
Coronavirus disease (COVID-2019) situation reports
U.S. situation reports from the U.S. Centers for Disease Control (CDC), updated most recently on March 15..
Also from the CDC:
From the CDC, a simple downloadable fact sheet with good basic information about the virus: Coronavirus disease 2019 (COVID-19) and you
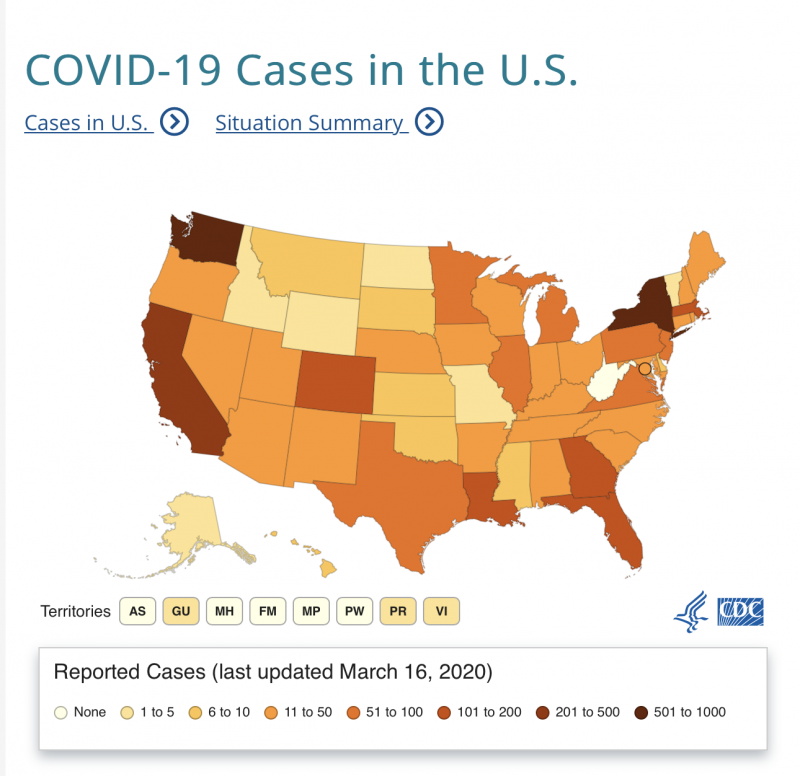
U.S. map showing number of coronavirus cases reported, state by state, as of March 16, 2020. Map via the CDC. (As of March 18, cases have occurred in all 50 states).
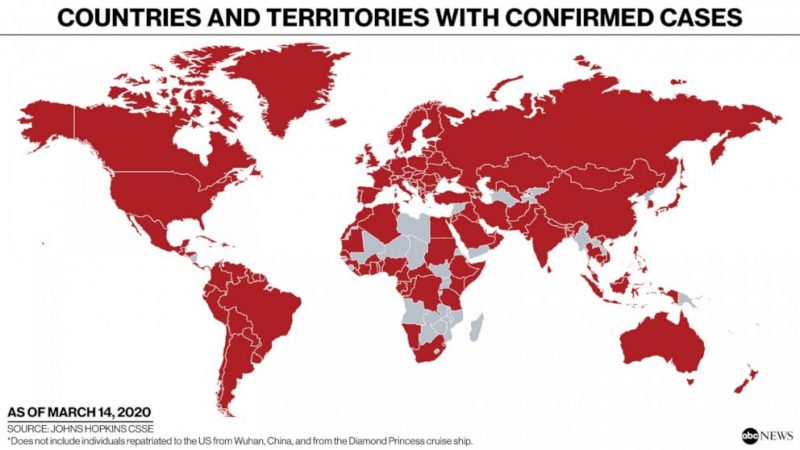
Countries and territories with confirmed cases of coronavirus, as of March 14, 2020. Read more from ABC News: Tracking the spread of coronavirus in the U.S. and around the world. Image via ABC News / Johns Hopkins CSSE.
Some background articles on the virus and its mitigation:
Why does soap work so well on the Sars-CoV-2, the coronavirus and indeed most viruses? Read more from chemist Pall Thordarson, via The Guardian: Here’s how soap kills the coronavirus
As the coronavirus spreads into more and more communities, public health officials are placing responsibility on individuals to help slow the pandemic. A physician explains how social distancing works. Read more from Thomas Perls, Professor of Medicine at Boston University: Why social distancing is the best tool to fight the coronavirus
More interesting threads from Twitter – March 15 and 16 – on the effect of coronavirus test shortages on doctors in the U.S., and how U.S. doctors are coping:
From @DrRobDavidson … Why testing is important from an emergency room doc’s perspective
From @Craig_A_Spencer … Another doctor’s comments, in New York City
From @Vivek_Murthy, who served as 19th Surgeon General in the U.S. … Another perspective (from March 13)
Last but not least, a good video on how social distancing works, using matches.

#StayHome. Image via @ASlavitt.
Bottom line: Links to information on coronavirus, updated March 18, 2020.
from EarthSky https://ift.tt/2UF0huy

Aucun commentaire:
Enregistrer un commentaire